Varicose veins are dilated, tortuous, enlarged veins. Any vein may become varicose, but the veins most commonly affected are those in your legs and feet. That’s because standing and walking upright increases the pressure in the veins of your lower body.
For many people, varicose veins and spider veins — a common, mild variation of varicose veins — are simply a cosmetic concern. For other people, varicose veins can cause aching pain and discomfort. Sometimes varicose veins lead to more-serious problems. Varicose veins may also signal a higher risk of other circulatory problems
The heart continuously pumps blood around the body to distribute nutrients and remove waste. The blood is taken away from the heart in arteries under high pressure passes through meshes of tiny blood vessels in the tissues (eg leg muscles) and is returned to the heart via veins which are thin walled collapsible tubes normally under relatively low pressure.
As veins are thin walled and collapsible the flow within them must rely on pumping from behind, rather than sucking from the heart in front as all this would achieve would be to collapse them.
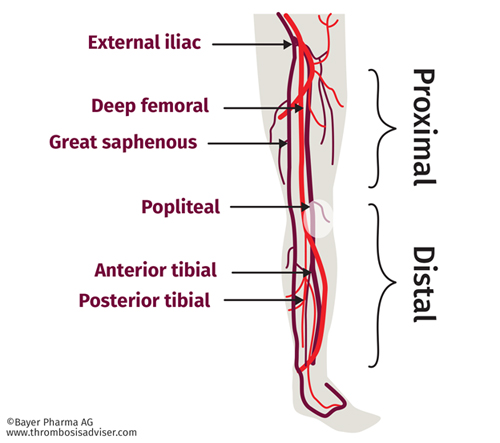
In the legs there are two main sets of large veins running parallel. The superficial (surface) system and the deep system. Blood in the superficial system flows into the deep system before being carried out of the leg up to the heart.
Humans spend a long time standing up and in this position the heart is about a metre or so higher than the veins in the lower leg. This makes it very difficult to get blood back to the heart from the legs. There are two main mechanisms which normally help the blood back up to the heart. First is the muscle pump in the calf. As the muscles contract they squeeze the blood out of the deep veins lying between them.
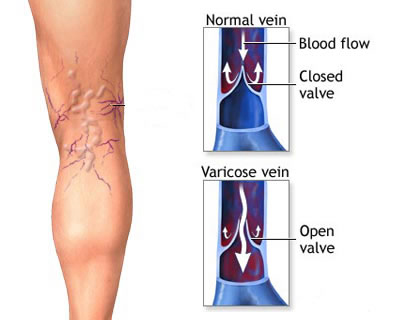
Some of this blood will tend to be squeezed up and some down. This is where the second mechanism comes in —- the valves in the veins which, when functioning, allow blood to flow upwards only.
Consequently in healthy legs when the muscles contract they squeeze blood out of the deep veins and as the valves stop it going down it all goes up in the direction of the heart. On relaxation of the calf muscles the pressure in the deep veins lowers and blood flows from the superficial into the deep system. There are also valves which stop blood flowing the wrong way from deep to superficial. Blood flow into the legs is nicely balanced by blood being pumped out and pressure in the veins is kept low.
Normal veins are largely invisible being either near the surface and very small or, if larger, much deeper. In thin or muscular people especially men there may be prominent but normal surface veins but these are easy to recognize cause no problems and require no treatment.
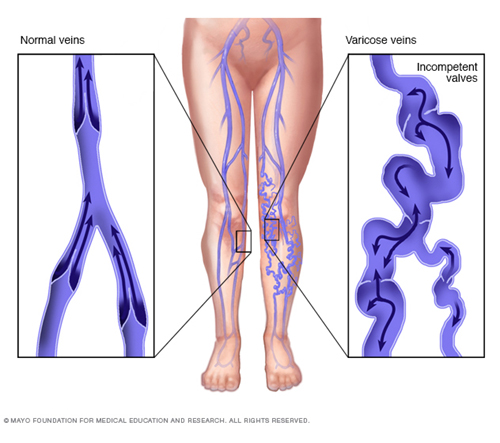
Varicose veins and spider veins are formed when this normal mechanism of venous blood flow fails. When the normal mechanisms of venous blood flow from the legs fail ‘venous insufficiency’ develops, which manifests in many ways. At its most mild venous insufficiency causes spider veins which are by and large cosmetic problems only, but can be associated with aching. Slightly larger bluey veins can also result which lie slightly deeper and are called reticular veins. More severe failure causes the common varicose veins and in 1-2% of the population over 65yrs and skin changes and ulcers will result.
All these are due to high pressure developing in thin walled veins which are designed to withstand low pressures only. Venous insufficiency can be caused by
- Deep vein obstruction
- Muscle pump failure
- Valve failure
Deep vein obstruction can be caused by DVT (Deep venous thrombosis) or by tumours in the pelvis compressing the veins. If it persists it causes valve failure too.
Muscle pump failure occurs in any condition where the calf muscles are very weak. If this persists it also causes valve failure. Poor muscle action in calves.
By far the commonest reason for venous insufficiency and varicose veins is valve failure which can result from inherited valve defects (most common); hormones (eg in pregnancy); trauma, previous thrombosis or weak calf muscles.
Once one valve is damaged allowing reflux through it this causes the vein below to stretch. This causes the next valve down to be pulled apart and also fail, leading to a domino type effect with more and more valves failing and eventually a varicose vein becomes prominent.
So you can see the most important factor is your genes; did your mother have varicose veins?
When the valves fail blood flows the wrong way through the veins away from the heart. This is called reflux. The detection, localisation and treatment of reflux is crucial to the effective management of all venous insufficiency problems including varicose veins, reticular veins, spider veins and ulceration.
 [/fusion_imageframe]
[/fusion_imageframe]
The most effective treatments for varicose veins are minimally invasive and guided by accurate medical imaging, including colour duplex ultrasound.
It is widely accepted that successful varicose vein treatment requires good imaging in the form of colour duplex ultrasound scanning to accurately map the anatomy (what the veins look like) and the physiology (how they are working eg. direction of blood flow). Even with the most innocent spiders it is important to check for valve failure and reflux as management of any sort of venous problem which neglects to detect and treat underlying reflux will fail. There may be short term success but the problem will recur and get worse.
Colour duplex ultrasound is a painless quick and non-invasive test. It is essential even in cases where reflux at the commonest site is detected clinically as the colour duplex test can detect other important features like further refluxing segments and variants of normal anatomy which may well alter the optimum treatment plan.
It is best if the doctor who is to undertake the treatment personally carries out the scan at the time of your consultation. This enables him to determine exactly what treatment is best and then be able to discuss and agree this with you.
As with the best traditional surgical techniques Interventional Radiological techniques aim to cure the problems by tackling the underlying cause. This entails elimination of the reflux and removal of incompetent veins and unsightly surfaced varicose veins.
This is most commonly achieved with surgery by tying the main superficial vein and its branches at the groin, stripping the main superficial vein and picking out any small unsightly varices which remain. This common operation though very successful and until recently widely accepted as the best treatment available is far from perfect. General anaesthesia and some hospital stay are required some complications like bruising, infection, scars, numbness etc can occur, time off work is necessary and the symptoms often recur.
interventional Radiological techniques also eliminate reflux and remove incompetent veins and superficial varices just like surgery but, by being performed under image guidance using microinstruments through tiny pinhole incisions, this is achieved as an outpatient, without anaesthetic cuts or scars, with excellent success rates and patient satisfaction and instant return to work and other activities.
The main difference in technique between our minimally invasive treatments and surgery is that in the latter the main superficial vein (great saphenous) is stripped out and removed altogether whereas in our methods the vein is totally destroyed ‘in-situ’ (where it lies). The outcome is the same but the destruction can be achieved very much more easily than the removal.
Interventional radiologists now use three main methods of vein destruction; Endovenous laser (EVLT), RF ablation and foam sclerotherapy. Although some doctors treat large veins by injections (foam sclerotherapy) the results are not as effective or as durable as either EVLT or RF ablation. Foam sclerotherapy is useful for any residual varicosities remaining at follow-up after either the EVLT or RF ablation treatment.
Both techniques rely on accurate preop mapping of anatomy and blood flow by colour duplex ultrasound and use of ultrasound to guide the instruments during the procedure.
You lie down on a couch with head up slightly the skin over your leg is cleaned with antiseptic solution and sterile drapes placed over your leg. A small injection of local anaesthesia will be given to numb the skin over the inside of your knee. A small sheath ( thin walled plastic tube ) is inserted into the vein to be destroyed usually just below the knee. Using an ultrasound image to guide the instruments the doctor then places a laser fibre or RF catheter through the sheath and up to the vein in the groin.
Local anaesthetic solution is then carefully injected around the vein along its whole length. The power is then turned on and the fibre/catheter slowly withdrawn. Once the length of the vein has been treated the sheath is withdrawn, a compression stocking will be applied and after a cup of tea you are allowed to leave, take a fifteen minute walk and get back to normal activities.

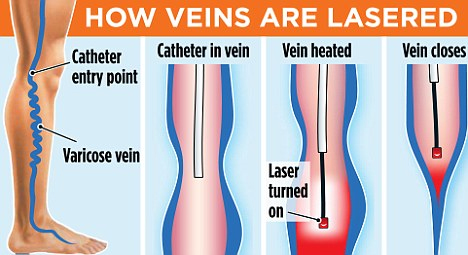
Over the next few weeks you may experience some tautness as the vein shrinks. You may also get some bruising but this is unlikely to be severe. You are asked to come back for assessment after 4-6 weeks. A check is made to see if the main vein is blocked as intended. If there are still any varicose veins remaining these are often small and symptomless but if you do feel they are unsightly then having dealt with the reflux we can simply ablate these remaining with an injection of a foam sclerosant or microavulsions under local anaesthetic. You need to wear compression stockings for two weeks following such treatment.

It has a number of benefits for patients:
- Rapid relief from symptoms.
- The imaging techniques allow accurate diagnosis and treatment using cutting-edge equipment. Diagnosis is reconfirmed during procedure.
- Minimally invasive procedures are performed through a small hole in the skin, minimising the patient’s discomfort and recovery time. There won’t be any scar.
- Most procedures can be performed on an outpatient basis or require only a short hospital stay. As interventional procedures tend to require only local anaesthesia, hospital stays are very short, with patients frequently going home the day the procedure is performed.
- Patients who undergo IR procedures experience less pain during and after the procedure than patients undergoing surgical procedures. Post-procedural care is provided, along with follow-up imaging to confirm if the treatment has been successful.
- Minimal damage to surrounding vital anatomical structures with no significant structural weakness.
- No or negligible blood loss. No requirement of blood transfusion.
- Return to work and other normal activities usually within the first few days after the procedure.
- Low risk compared to surgery. The techniques can be used in very sick patients who are unfit for surgery.
- Overall procedure is less expensive than surgery or other alternatives.
