With a diameter of less than 1 mm, spider veins are the miniature versions of varicose veins. The dilated, small veins lie within the skin and not beneath it like the large varicose veins. For this reason, the spider veins can be seen shimmering clearly through the skin, particularly in fair-skinned people. They can be found anywhere on the leg, but appear particularly frequently on the outer side of the lower leg and thigh and the inner side of the knee.
Spider veins may be bluish or reddish-purple in color and have a dotted, stripy, fan-shaped, or star-like (starbursts) appearance. They may occur singly or in clusters and, in the worst cases, extend over a relatively large area on the leg.
Spider veins are usually considered to be purely an aesthetic problem, but they may be the first visible sign of venous insufficiency that will become worse with time. Pronounced spider veins may cause symptoms and may indicate that larger varicose veins are already present and possibly even be the cause of the spider veins.Spider veins may occur on their own or together with large varicose veins. Spider veins may also be very pronounced: in the case below, the spider veins are due to a diseased perforating vein(perforator) connecting the systems. This vein also needs to be treated as it is supplying the spider veins with blood.
A particularly severe form of spider veins on the foot is called corona phlebectatica. These spider veins are considered to be an early sign of advanced vein disease. A person with this condition should see a doctor without delay.

These small networks of varicose veins lie somewhat deeper in the skin than spider veins, but they often occur together and are frequently interconnected. Reticular varicose veins have a diameter of 1-3 mm and are slightly larger than spider veins. With their bluish or greenish-blue colour they are clearly visible.
Reticular veins tend to form a fan-like or netted appearance and, like spider veins, are often found on the sides of the upper and lower leg.
In technical language, both spider veins and reticular veins are classified together in one group as C1 varicose veins. C1 covers the mildest form of varicose disease, generally considered as a cosmetic problem rather than a medical one.
The most noticeable sign of spider veins is their appearance on the skin. In most cases, there are no symptoms present and spider veins are considered to be harmless and not usually considered a health risk. But on occasion they have been known to have some minor symptoms which might include things like:
- Restless legs or uncomfortable legs
- A rash
- Aching, cramping or throbbing legs
- Itching around the vein sites
- Skin ulcers
- Swelling
It’s important to seek medical attention if the veins feel warm to touch or are tender; or if you develop ulcers or sores on the skin.
Millions people in the world have either spider veins or varicose veins
About half of the women who are between 40 and 50 years of age have spider veins; and 75% of the women who are between 60 and 70 years old have them. About half of the men over 70 have spider veins and one fourth of men who are between 30 and 40 have spider veins.
Spider veins result when the valves in the veins become weak or damaged. If the valves cannot or do not open up properly to allow blood to freely flow in and out, blood starts to back up and the veins will swell. There can be several factors that increase the risk of developing the condition. Examples include:
- Getting older
- Family history of spider veins
- History of blood clots
- Birth control pills
- Pregnancy
- Wearing clothing that is too tight
- Obesity
- Constipation
Which treatment option works best for you will be determined by your specific condition and preferences.Conservative treatment is helpful in asymptomatic patients in early stages. Laser treatments typically have fewer side effects and are less painful than Sclerotherapy. However, Sclerotherapy works better in cases where the veins are a little deeper and the laser cannot be used. Recovering from laser treatments is immediate and there is absolutely no down time involved. Laser treatments can also be used on spider veins that occur in the facial area. But, laser treatments are often more expensive than Sclerotherapy.
1. Conservative treatment of spider veins
Conservative treatment for chronic vein disease includes compression therapy and medication. Some experts also count sporting activities and vein training as conservative treatment methods.
Although they serve to relieve the symptoms, none of these conservative measures actually eliminates spider veins. Conservative treatment is therefore usually employed as preventive measure or to support other forms of treatment.
- Compression therapy
As a rule, compression therapy is used for large varicose veins and plays a more minor role in treating spider veins – even though compression stockings can improve the blood flow in spider veins as well.
- Medication in the treatment of spider veins
Vein products are available in the form of sprays, ointments, and gels to be applied to the skin or as tablets and capsules to be taken by mouth. The effects of most vein products for external use have not been proved scientifically, so their use remains controversial. Promises made by some products that spider veins will disappear with regular use, should be viewed with caution, because it is a fact that once spider veins have appeared, they will not go away without treatment from a doctor.
Oedema-protective agents are worthwhile. Oral vein products such as oedema-protective agents certainly make a lot of sense in vein disease – they demonstrably relieve symptoms in the legs and reduce the accumulation of fluid in the tissues. With varicose veins, the vein walls are more permeable to components of the blood. As a result, abnormal quantities of fluid collect in the tissues (oedema). Studies have shown that oedema-protective agents reduce the pathological (abnormal) permeability of the vein wall and counteract fluid accumulation. These agents are most effective when taken prophylactically, i.e. before the oedema develops.
When spider veins cause symptoms, these vein tablets may relieve the complaints.
Oedema-protective agents are available at pharmacies and have been used traditionally to relieve the feelings of heaviness and swelling in the legs.
Nevertheless, these oedema-protective agents cannot eliminate spider veins either and, as a general rule, they cannot and should not replace other preventive measures or professional medical treatment.
2. Sclerotherapy of spider veins
Elimination of spider veins with sclerotherapy. Sclerotherapy is the overall term used to describe the method when it is used for varicose veins of any type; the treatment of spider veins and small varicose veins is called micro-sclerotherapy. The prefix ‘micro-’ indicates that the small veins are treated with extremely fine needles. The aesthetic appearance is of prime importance in the treatment of spider veins. Micro-sclerotherapy is an outpatient procedure and can eliminate spider veins without the need for lasers, anaesthetics, and incisions.
- Effective and safe
- Relatively painless
- No possible scarring due to heat
- Cost-effective
- Very good evidence from clinical studies
- Treatment of choice according the therapeutic guidelines
- Can be used to treat all types of varicose vein
Disadvantages of micro-sclerotherapy
- Allergies and systemic reactions are possible in rare cases
- Requires injections with a fine needle
- Compression stockings are recommended for a few days
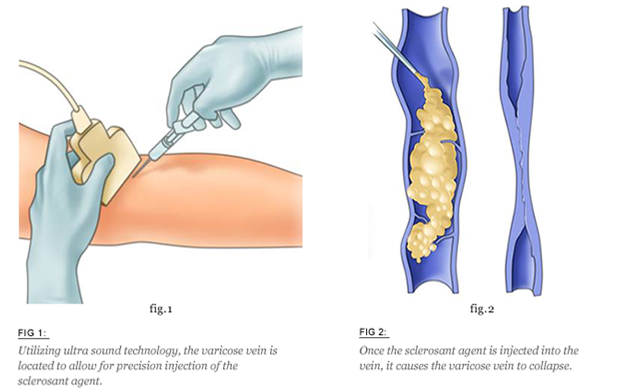
How micro-sclerotherapy works
In micro-sclerotherapy, the doctor uses a very fine needle to inject a specially developed medicinal product, the sclerosant, directly into the spider veins and small varicose veins. Inside the diseased vein, the sclerosant reacts with the vein wall. Natural processes cause the walls to stick together, thus closing off the diseased vein. The body gradually converts this vein into a strand of connective tissue by a process known as sclerosis. With time, the connective tissue strand is gradually broken down until it finally disappears.
Foam sclerotherapy of spider veins
Foam sclerotherapy involves the injection of special sclerosant foam into the spider veins instead of a liquid sclerosant.
According to the European guidelines on the sclerotherapy of varicose veins, micro-sclerotherapy with liquid sclerosant is still the method of choice for treating spider veins and small varicose veins. However, these guidelines also list foam sclerotherapy as an alternative method for treating spider veins, with a similar rate of success and range of side effects.
3. Laser therapy of spider veins
In principle, spider veins on the legs can also be treated with a particular type of laser (Nd:YAG laser). However, laser therapy is only successful when the spider veins are small, not very pronounced, and when there is no inflow from deeper-lying veins. The reason for such limitations is that the penetration depth of laser beams is not sufficient to reach and obliterate any deeper-lying diseased veins. For effective treatment, however, it is essential to treat these more deeply lying veins as well, because the spider veins will otherwise reappear again and again.
Advantages of laser therapy
- Acts through the skin without any injections
- Compression stockings are not recommended
- Fewer systemic reactions
Disadvantages of laser therapy
Often ineffective; the penetration depth is not sufficient to reach reticular varicose veins
Can only be used to treat fine, small spider veins without an inflow from deeper-lying veins
- No adequate studies
- Painful
- Scarring is more common
- Heat damage is possible
- Cooling is necessary
- Treatment is not recommended in the guidelines
- More expensive
- Often needs to be combined with sclerotherapy for optimal success
How laser therapy works
Laser beams are electromagnetic waves that strike human tissues as strongly bundled beams emitted from the laser device. Depending on the duration and intensity of the exposure, the thermal effects that can be seen range from slight warmth to charring of the tissues.
When the laser beam penetrates to a sufficient depth, haemoglobin (which gives the blood its red colour) in the spider veins absorbs the laser light and converts this energy into heat. The blood is sort of boiled and clots. The thermal action damages the inner layer of the vein walls and causes them to stick together at these points. However, the effects of laser therapy are seen only at the points where the bundled beams meet the tissues. This means that, under cooling, the skin of the spider veins must be (repeatedly) treated with the laser at intervals along their entire length; the points of application have to overlap in order to obliterate the whole blood vessel. If the overlap is too great, the heat generated may damage the skin. If the points of application are too far apart, the diseased vein may not stick together along its whole length, leaving open segments of the vein filled with blood. Parts of the spider vein will then remain visible.
Successful laser therapy results in the formation of a connective tissue strand that is resorbed into the body after a few weeks or months.


