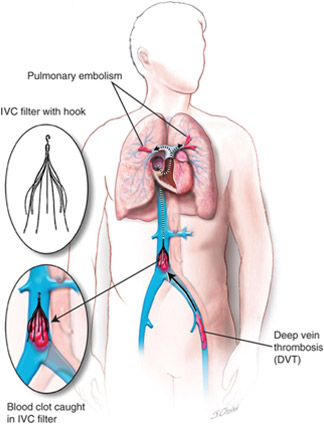
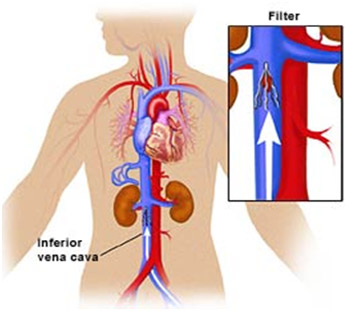
In an inferior vena cava filter placement procedure, interventional radiologists use image guidance to place a filter in the inferior vena cava (IVC), the large vein in the abdomen that returns blood from the lower body to the heart.
Blood clots that develop in the veins of the leg or pelvis, a condition called deep vein thrombosis (DVT), occasionally break up and large pieces of the clot can travel to the lungs. An IVC filter is a small metal device that traps large clot fragments and prevents them from traveling through the vena cava vein to the heart and lungs, where they could cause severe complications such as pain, difficulty breathing, shortness of breath or even death.
Until recently, IVC filters were available only as permanently implanted devices. Newer filters, called optionally retrievable filters, may be left in place permanently or have the option to potentially be removed from the blood vessel later. This removal may be performed when the risk of clot travelling to the lung has passed. Removal of an IVC filter eliminates any long term risks of having the filter in place such as filter fracture or recurrent DVT. It does not address the cause of the deep vein thrombosis or coagulation. Your referring physician will determine if blood thinners are still necessary. However, not all retrievable IVC filters are able to be retrieved if the risk of clots traveling to the lung persists. These filters can be left in place as permanent filters.
Inferior vena cava (IVC) filters are placed in patients who have a history of or are at risk of developing blood clots in the legs, including patients:Inferior vena cava (IVC) filters are placed in patients who have a history of or are at risk of developing blood clots in the legs, including patients:
- Diagnosed with deep vein thrombosis (DVT).
- With pulmonary embolus.
- Who are trauma victims.
- Who are immobile.
- Who have recently had surgery or delivered a baby.IVC filters are used when patients cannot be successfully treated by other methods, including blood thinning agents.
Prior to your procedure, your blood may be tested to determine how well your kidneys are functioning and whether your blood clots normally.
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to local anesthetic medications, general anesthesia or to contrast materials containing iodine (sometimes referred to as “dye” or “x-ray dye”). Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners for a specified period of time before your procedure.
Also inform your doctor about recent illnesses or other medical conditions.
Women should always inform their physician and x-ray technologist if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the fetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby. See the Safety page for more information about pregnancy and x-rays.
You should eat a light meal the night before your procedure.
You will likely be instructed not to eat or drink anything after midnight before your procedure. Your doctor will tell you which medications you may take in the morning.
You may be allowed to drink clear liquids on the day of your procedure.
If you are diabetic and take insulin, you should receive instructions on eating and insulin dose from the interventional radiologist, as your usual insulin dose may need to be adjusted on the day of the procedure.
You may be asked to remove some or all of your clothes and to wear a gown during the exam. You may also be asked to remove jewelry, eye glasses and any metal objects or clothing that might interfere with the x-ray images.
You should plan to have a relative or friend drive you home after your procedure.
Using image guidance, a catheter is inserted through the skin into a large vein in the neck or upper leg and advanced to the inferior vena cava in the abdomen. The IVC filter is then placed through the catheter and into the vein. Once it is in the correct position, the interventional radiologist will release the filter, allowing it to fully expand and attach itself to the walls of the blood vessel.
To remove an IVC filter, a special catheter is inserted into a large vein in the neck or groin and advanced to the site of the filter in the vena cava. A removable IVC filter has a small hook or knob at one end that enables the catheter to capture the filter, close it, pull it into the catheter and then withdraw it from the body.
Image-guided, minimally invasive procedures such as inferior vena cava filter placement and removal are most often performed by a specially trained interventional radiologist in an interventional radiology suite or occasionally in the operating room.
This procedure is often done on an outpatient basis. However, some patients may require admission following the procedure. Please consult with your physician as to whether or not you will be admitted.
You will be positioned on your back.
You may be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm so that sedative medication can be given intravenously. Moderate sedation may be used. As an alternative, you may receive general anesthesia.
The area of your body where the catheter is to be inserted will be sterilized and covered with a surgical drape.
Your physician will numb the area with a local anesthetic.
A very small skin incision is made at the site.
Using image-guidance, a catheter (a long, thin, hollow plastic tube) is inserted through the skin to the treatment site.
Contrast material may be injected into the inferior vena cava to help guide the catheter and verify precise placement of the IVC filter in the blood vessel.
At the end of the procedure, the catheter will be removed and pressure will be applied to stop any bleeding. The opening in the skin is then covered with a dressing. No sutures are needed.
Your intravenous line will be removed.
The procedure is usually completed within one hour.
Devices to monitor your heart rate and blood pressure will be attached to your body.
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line (IV) and when the local anesthetic is injected. Most of the sensation is at the skin incision site which is numbed using local anesthetic. You may feel pressure when the catheter is inserted into the vein or artery.
If the procedure is done with sedation, the intravenous (IV) sedative will make you feel relaxed, sleepy and comfortable for the procedure. You may or may not remain awake, depending on how deeply you are sedated.
You may feel slight pressure when the catheter is inserted, but no serious discomfort.
As the contrast material passes through your body, you may experience a warm feeling which quickly subsides.
You will remain in the recovery room until you are completely awake and ready to return home.
If your IVC filter was inserted through a vein in your neck, you should be able to resume your normal activities within 24 hours. If your filter was inserted through a vein in your groin, you should avoid driving for 24 hours and lifting heavy objects and climbing stairs for 48 hours. Your physician may provide additional post-procedure instructions.
The interventional radiologist can advise you as to whether the procedure was a technical success when it is completed.
Your interventional radiologist may recommend a follow-up visit after your procedure or treatment is complete.
The visit may include a physical check-up, imaging procedure(s) and blood or other lab tests. During your follow-up visit, you may discuss with your doctor any changes or side affects you have experienced since your procedure or treatment.
Benefits
- No surgical incision is needed—only a small nick in the skin that does not have to be stitched.
- The filter has a high rate of success in protecting lungs from serious pulmonary embolus (PE) in patients who have failed conventional medical therapy or cannot be given conventional medical therapy.
Risks
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
- There is a very slight risk of an allergic reaction if contrast material is injected.
- Any procedure that involves placement of a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel, bruising or bleeding at the puncture site, and infection. However precaution is taken to mitigate these risks.
- There is a chance that the IVC filter can lodge in the wrong place, change position or penetrate through the vein (which can rarely lead to injury of a nearby organ).
- The IVC filter or a piece of the IVC filter may break loose and travel to the heart or lungs causing injury or death.
- Rarely, IVC filers become so filled with clots that they block all flow in the blood vessel, causing swelling in the legs.
- In some cases, retrievable filters become scarred to the vein and cannot be removed, in which case they are left in permanently (as they are also designed to do).
