A permacath is a piece of plastic tubing – very similar to a jugular catheter – and is used inexactly the same way for your haemodialysis.
The permacath has a cuff that holds the catheter in place and acts as a barrier to infection. Thecuff is underneath the skin and cannot be seen. The catheter part that you can see is the partthat protrudes from the chest wall. It is about 6 inches/15cms long and is made of soft, white, flexible plastic. There are 2 limbs.
A transparent dressing will be put over the part where the catheter leaves the chest wall and(since the catheter is under the level of your collar bone) it will not be seen when you areclothed.
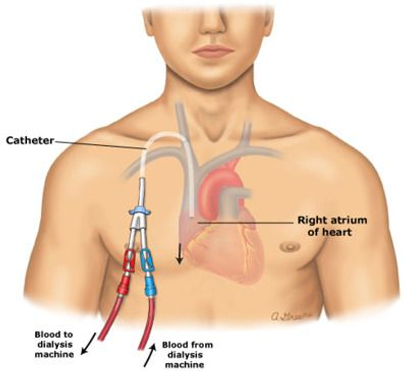
The permacath is placed in the jugular vein. It is tunnelled under the skin and tissues along theupper chest, under your collar bone and the end of the catheter will come out on the chest wall,about 4 inches/10cms underneath the collar bone.
As the permacath is less prone to infection, it can remain in your body for longer than thejugular catheter, whilst you are waiting for a fistula to be inserted. Occasionally, it is used forlonger if a fistula cannot be formed. However, infections can occur in the permacath and itsometimes needs to be replaced.
During the procedure, x-rays are used to ensure that the permacath is being placed in the bestposition.
You will be given some sedation through the drip. This will make you relaxed and sleepy, bothduring the procedure and during the rest of the evening.
The medical staff will be wearing green gowns and gloves. This clothing is needed in order tomaintain a sterile environment during the procedure, which minimises infection.
A clip will be placed onto one of your fingers in order to monitor the oxygen levels in the bloodduring the procedure. The machine makes a bleeping noise.
Once the sedation has taken effect the permacath is tunnelled underneath the skin into thejugular vein. You will have 2 – 3 stitches at the bottom of your neck and the catheter will comeout of your chest wall.
There will be another stitch around the catheter, where it leaves your chest wall. A transparentdressing will be put on both those areas and the stitches will be removed in 10 days by theRenal Unit or ward staff.
There is a small risk (as with a jugular catheter) of puncturing the lung. Therefore, if you experience excessive pain or shortness of breath when you return to the ward, it is important for you to tell the ward staff immediately.
There is also a small risk of bleeding from the permacath site, and it may be necessary for you to have an extra stitch put in to stop any more bleeding.
As with the jugular catheter, there is a risk of infection. In order to minimise this risk, staff wear gloves and use sterile supplies when connecting and disconnecting you to and from the dialysis machine.
Your temperature will be checked each time you come to dialyse and the dressing will be checked for any signs of infection underneath it. It is also important that you inform the Renal Unit staff of any pain, redness or leakage that you may see from the site of the catheter. The dressing is changed at least once a week.
If you are concerned about these risks or have any further queries, please speak to your consultant.
Your consultant has recommended this procedure as being the best option. There are no alternative procedures available. However, there is always the option of not receiving any treatment at all. The consequences of not receiving any treatment are potentially life threatening. If you would like more information please speak to your consultant or one of the nurses caring for you.
You will feel sleepy for several hours. You may feel some discomfort around the permacath and have some bruising. This is to be expected and pain relief may be necessary – please inform the ward staff if you are in discomfort or pain. During the procedure a small amount of blood is lost. This is unavoidable. You will have some blood on the back of your head and neck when you wake up. This looks more than it is, so please don’t be alarmed.
If everything has gone well, you will be able to go home the next day. Your catheter is to be treated as you treated your jugular catheter. An information sheet will be given to you when you leave hospital.
