Venography demonstrating more than 50% stenosis of the subclavian, brachiocephalic vein, and superior vena cava in the upper extremity or the iliac vein or inferior vena cava in the lower extremity is considered central venous occlusion.Central venous occlusion occurs commonly in hemodialysis patients. It should be suspected when there is unilateral edema of the extremity ipsilateral to an existing or previous tunneled dialysis catheter.
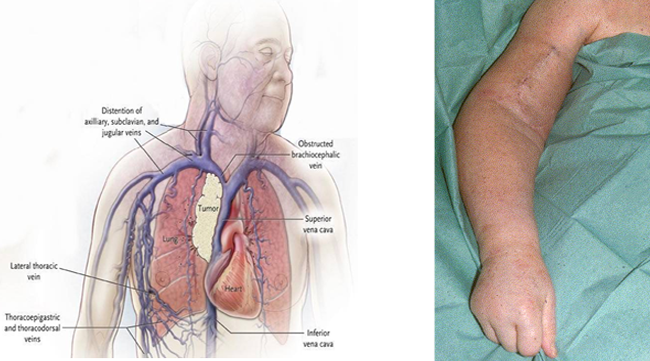
In the majority of patients central vein obstruction is due to previous inserted central vein catheters. In 40% of the patients with subclavian vein catheters central venous obstruction develops, compared with 10% of patients with jugular vein catheters. In patients without a history of central venous catheterization, other causes, such as extrinsic compression of mediastinal veins (e.g. lymphoma, goitre, thoracic aortic aneurysm, mediastinal fibrosis, pacemakers), hypercoagulopathy, thoracic outlet syndrome or pacemaker wires should be considered.
Chronic swelling of the access arm is the most important clinical sign of central venous obstruction.
The superficial veins may become prominent (collaterals).
Pain and paraesthesia may occur.
In obvious central venous obstruction, angiography of the access and complete venous outflow tract must be performed, since the central veins cannot be examined with ultrasonography.
Thus, to completely visualize all mediastinal veins, venography using digital subtraction technique is needed. This can be done preferably with direct antegrade puncture of the access.
In cases of extrinsic obstruction of central vein plain X-rays, computed tomography or MR imaging may be helpful for the differential diagnosis.
Your Content Goes HereCentral venous lesions have to be treated when they are severe and disabling such as those resulting in arm swelling, troublesome pain or inadequate haemo-dialysis. If treatment of the underlying disease is not possible or fails to resolve arm swelling, PTA with stent insertion is indicated.
Interventional treatment
Percutaneous transluminal angioplasty with or without stent implantation is recommended as primary option for treatment. Reports show, that symptomatic central venous obstruction in dialysis patients can be treated with a high success rate through radiological intervention.
Stent placement should avoid overlapping the ostium of a patent internal jugular vein to achieve a safe and sufficient result, since this latter vein is essential for future placement of central venous catheters. Similarly, a stent placed in the innominate vein should not overlap the ostium of the contralateral vein, otherwise contralateral stenosis may occur and preclude future use of the contralateral limb for access creation. Little data are available on the useof thrombolytic agents in central venous thrombosis. It is, therefore, not recommended as a primary treatment regimen.
Regular follow-up and repeat interventions are required to maintain patency and achieve long-term clinical success.
Surgical treatment
Surgical reconstruction of mediastinal veinsand Extra-anatomical bypass are rarely done due to significant associated risk. Closing dialysis fistula in the affected limb can be done if all options fail.
