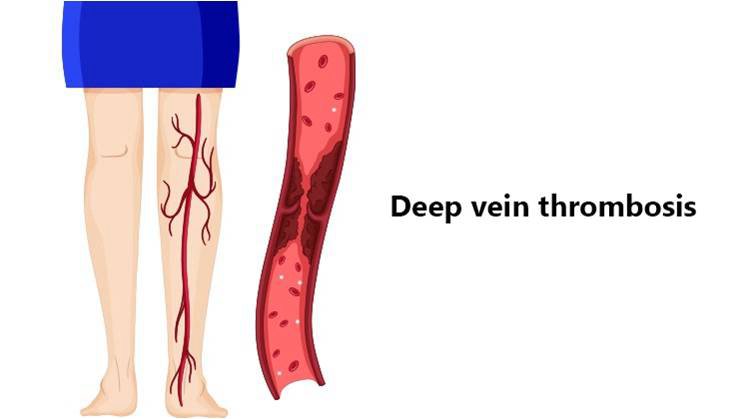
Deep vein thrombosis (DVT) is a condition in which a blood clot develops in one of the primary veins of the pelvis, thigh, or calf, or less frequently the arms, abdomen, and chest. When a clot forms, it can extend to adjacent areas of the vein, triggering a localized inflammation that may encourage additional blood clot growth. A clot in a deep vein can also increase the potential for a dangerous complication, pulmonary embolism, in which a clot breaks free, travels through the bloodstream, and lodges in the lungs, where it can cause heart and lung collapse.Lower extremity deep venousdisease is the third most commoncardiovascular disease and is associatedwith significant individualmorbidity and high societal cost.
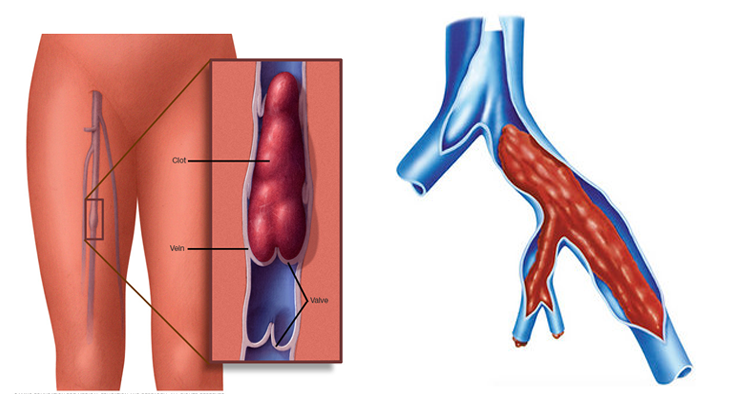
Deep vein thrombosis signs and symptoms can include:Swelling in the affected leg. Rarely, there’s swelling in both legs.
-
Pain in your leg. The pain often starts in your calf and can feel like cramping or soreness.
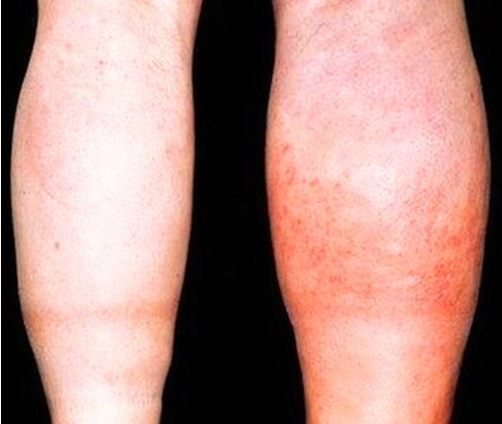
- Red or discolored skin on the leg.
- A feeling of warmth in the affected leg.
Deep vein thrombosis can occur without noticeable symptoms.The warning signs and symptoms of a pulmonary embolism include:
-
Sudden shortness of breath
-
Chest pain or discomfort that worsens when you take a deep breath or when you cough
-
Feeling lightheaded or dizzy, or fainting
-
Rapid pulse
-
Coughing up blood
Risk factors for DVT include:
- recent trauma
- major surgery
- cancer
- paralytic stroke
- estrogen treatment (birth control pills)
- immobilization
- obesity
- increased age, and history of previous clotting problems in the patient or family
The most common test for diagnosing deep vein blood clots is Colour duplex ultrasound. It is a painless quick and non-invasive test. It is best if the doctor who is to undertake the treatment personally carries out the scan at the time of your consultation. This enables him to determine exactly what treatment is best and then be able to discuss.
Sometimes MR Venography is required to know extent of disease and May-Thurner syndrome. May-Thurner syndrome is a clinical entity of left iliac vein compression by the right iliac artery, resulting in isolated left lower extremity swelling and may be a precipitating factor for iliofemoral deep venous thrombosis. Magnetic resonance imaging is the best modality for diagnosis of this entity as it can rule out the presence of pelvic masses and deep venous thrombosis while simultaneously demonstrating the anatomy characteristic of this syndrome.
Conventional Deep vein thrombosis treatment options include:
- Blood thinners. Deep vein thrombosis is most commonly treated with anticoagulants, also called blood thinners. …
- Compression stockings.
Endovascular treatment for Deep vein thrombosis include:
Acute DVT: Pharmacomechanical catheterdirectedtherapy (PCDT)
Chronic DVT: Stent placement in Iliofemoral or large veins in the setting ofchronic thrombotic and nonthromboticdeep venous diseasehas shown good long-term clinicaloutcomes.
- Stand-alone anticoagulant therapy fails to prevent Post thrombotic syndrome in a significant proportion of patients with acute proximal DVT, leading to significant disability, quality of life impairment, and socioeconomic costs
- Patients with iliofemoral DVT are at particularly high risk for Post thrombotic syndrome and late disability.
- Treatment strategies that feature early thrombus removal may prevent Post thrombotic syndrome
- CDT has significant potential toprevent Post thrombotic syndrome and offers distinct advantagescompared with surgical venousthrombectomy, systemic thrombolysis,and anticoagulation alone.
- Adjunctive CDT is likely to providefaster symptom relief than anticoagulationalone and does not increasethe risk of symptomatic PE.
PTS is a chronic conditiondefined as a set of symptoms andsigns that develop in a limb months toyears after an acute DVT. These includedaily limb pain and/or aching, fatigue,heaviness, and/or swelling that worsenswith upright position and activity. In severelyaffected patients, limiting venousclaudication, stasis dermatitis, subcutaneous
fibrosis, and/or skin ulcerationmay develop.
Pharmacomechanical Catheter Directed Thrombolysis (PCDT) includes combined use of Catheter directed thrombolysis and catheter-based suction or mechanical thrombectomy.
Thrombolysis is a minimally invasive procedure in which we administer clot-dissolving drugs directly into the clot to break it up. During thrombectomy we use a catheter tipped with a tool that mechanically breaks up the clot or remove clot by catheter suction. These two procedures are sometimes used together, and are useful for very large clots or in people who are at high risk of developing a pulmonary embolism. Patients also receive anticoagulation before, during, and after endovascular treatment.
On the night before the procedure eat a light meal, then do not eat or drink anything after midnight. We will provide you with more detailed information about which medications you may take in days before and on the morning of the procedure. Plan to have someone drive you home after the procedure.
After you arrive at the interventional radiology suite and change into a gown, you will lie on the procedure table. To relax you and block any pain we will intravenously give you a combination of medicines called “conscious sedation.” Using X-ray and/or ultrasound image guidance, we will insert a long, very thin tube called a catheter into a small hole in a vein either below your knee or in your groin and thread it through the vein to the clot.
Using a catheter equipped with holes along the sides we will release a clot-dissolving (thrombolytic) drug directly into the clot to dissolve it, and in some cases will also mechanically break up the clot using a catheter tipped with a tiny metal coil. Once the clot is removed with suction catheter we will withdraw the catheter and close the hole. This procedure takes about one to three hours.
The most common complications of thrombolysis and thrombectomy include bleeding from the needle puncture. Other complications include low blood pressure, an allergic reaction to the clot-busting medication, post-thrombotic syndrome (swelling, pain, and ulcers (sores), or, very rarely, Intracranial hemorrhage (bleeding in the brain tissue).
After the procedure we will have you rest in the recovery area, and we will give you intravenous fluids, antibiotics to prevent infection, and painkillers to relieve discomfort at the catheter insertion site. We may discharge you once any bleeding from the venous puncture site has stopped and your vital signs are normal.
